Series 1: Scout
The scout is acquired as a free-breathing half-Fourier acquired single-shot turbo spin echo (Siemens HASTE) or single-shot fast spin echo technique (GE SSFSE). During this 25-s scan, 28 slices are acquired: 8 in the sagittal plane, 5 in the coronal plane, and 15 in the axial plane.
Series 2: Coronal T2 breath-held
In addition to its role as a screen for pathology, this series can be used as a reference for prescribing subsequent breath-held sequences. HASTE or SSFSE is typically the default sequence, allowing complete chest coverage in a single breath-hold. If further detail is desired, a 2D multislice multibreath-hold turbo spin echo (Siemens TSE) or fast spin echo (GE FSE) can be employed. We currently use a periodically rotated overlapping parallel lines with enhanced reconstruction (PROPELLER) technique acquired in about 5-6 breath-holds of about 17-23 s. BLADE is the Siemens proprietary variant of PROPELLER. We have found that the central k-space oversampling and inherent motion correction properties of this technique result in less motion artifact from the heart and subtle respiratory modulations as well as increased sharpness of the lung/pleural interface. Analogous observations in the pelvis have been reported. [8] Radial artifacts can be minimized by appropriate attention to blade width and oversampling parameters.
Series 3: Coronal 2D bSSFP, free-breathing
This series is a nonfat-saturated 2D multislice balanced steady state free precession (bSSFP) sequence. These image acquisitions are often extremely useful, providing exquisite anatomic information and soft tissue contrast as well as dynamic information on diaphragmatic excursion with respiration. Occasionally, relative tumor mobility can be assessed on these image acquisitions. This 2D technique of evaluating lung motion in both healthy volunteers and in patients with intra- and extra-pulmonary disease has been compared with other investigational 3D MRI techniques [9] with reported good correlation. In patients who cannot receive intravenous gadolinium, bSSFP images often provide an adequate look at the central vascularity.
Series 4: Navigator scout
The purpose of this series is to optimize placement of a 2D navigator for subsequent navigator-triggered acquisitions. Navigator Scout images are HASTE/SSFSE acquisitions, which, at first glance, may seem like a redundant series to the Scout Series. We have observed that: (1) initial anxiety can lead to erratic diaphragmatic motion, which is generally allayed this far into the examination, making tracking of the right hemi-diaphragm more regular at this point of the examination, and (2) we can obtain a more reliable location of the posterior aspect of the dome of the liver on an axial slice, which is an optimal place for navigator placement. Some patients who have had surgery on the right side may have suboptimal right hemi-diaphragmatic excursion, and in those instances, we have been successful in placing the navigator on the left hemi-diaphragm at the level of the spleen.
Series 5: Axial T2 navigator-triggered
We have found T2 TSE BLADE/PROPELLER to be qualitatively comparable to, if not favored over, conventional T2 TSE acquisitions, particularly given the reduced sensitivity to cardiac motion and increased sharpness of the major tissue interfaces. Fat saturation is routinely employed for this series. In addition to lesion characterization, this sequence is highly useful for the evaluation of lymphadenopathy and regional bone marrow signal.
Series 6: Axial diffusion-weighted imaging, respiratory-triggered
For this 2D multislice echo planar imaging (EPI) respiratory-triggered acquisition, we have selected b values of 0, 100, and 800 s/mm 2 . Diffusion-weighted imaging (DWI) in other body systems has provided information suggesting the cellularity of the lesion of interest and, because of this, is of particular interest as a potential biomarker of disease and treatment response. To obviate any T2* effects that could be induced in the lesion due to gadolinium, we have decided to perform DWI prior to contrast administration. Further investigation is needed to determine if "pseudoperfusion" (intravoxel incoherent motion) effects elucidated by using lower b-values (less than 100 s/mm 2 ) provide additional clinically relevant information.
Series 7: Pregadolinium T1 3D SPGR
A variety of 3D T1-weighted fat-saturated gradient recalled echo (GRE) sequences are available. Currently, we use a 3D spoiled gradient recalled (SPGR) with accelerated parallel imaging acquisition technique (Siemens VIBE with CAIPIRINHA or GE LAVA-Flex with Auto-calibrating Reconstruction for Cartesian (ARC) sampling and Dixon method for fat suppression, repition time/echo time TR/TE (3.82/1.8 ms), and matrix/slice thickness (256 × 256)/3 mm. In- and -out-of-phase images are routinely reconstructed. Homogeneous fat saturation of the anterior-superior mediastinum near the origin of the great vessels can be challenging with non-Dixon methods and particular attention to manual shim boxes is helpful in this regard.
Series 8: Test bolus
For this portion, repeated real-time single-slice GRE axial acquisitions at the level of the pulmonary artery are acquired following injection of 1 cc of intravenous contrast followed by a 20 cc normal saline flush. The time to peak enhancement in the pulmonary artery or ascending aorta can be determined.
Series 9: Postgadolinium T1 3D SPGR
Using the information from the test bolus, the initial postgadolinium series is timed such that peak arterial enhancement coincides with the time of central k-space filling. Identical parameters are used for the pre- and postgadolinium series, with images typically acquired in the axial plane. Subsequent postgadolinium images are typically obtained at 1, 3, and around 5 min. An additional imaging plane, either coronal or sagittal, is often obtained.
Series 10 (optional): T1 SPGR breath-held In- and out-of-phase
The information provided by this dual-echo 2D GRE sequence with respect to the presence of intravoxel fat is particularly useful in imaging anterior mediastinal masses where the normal or hyperplastic thymus is a consideration. [10] The imaging parameters are Repetition Time/First Echo Time/Second Echo Time (TR/TEΉ/TE) (170/2.38/4.76 ms), matrix/slice thickness (256 × 192)/5.5 mm. In practice, we have found the in- and out-of-phase images obtained from the pregadolinium T1 3D SPGR with Dixon technique can be comparably used, thus saving the time associated with running a separate two-dimensional T1-weighted Gradient-Recalled Echo (2D T1 GRE) for this purpose.
Series 11 (optional): Axial bSSFP breath-held
The 2D bSSFP (Siemens TRUE FISP or GE FIESTA) technique demonstrates T2/T1-weighting with high contrast and signal-to-noise ratio and can be obtained with rapid sequential acquisition, fat suppression, and overlapping thin sections. It is frequently used in cardiac and abdominopelvic MRI as a noncontrast-enhanced bright blood MR angiography/venography technique. These are typically performed as breath-held acquisitions but can be tailored to be free-breathing.
Series 12 (optional): Cine bSSFP
CinebSSFP (Siemens TRUE FISP or GE FIESTA) is a staple of cardiac imaging for the evaluation of cardiac wall motion, function, and valves. In the context of noncardiac chest MRI, this technique is useful for evaluating the motion of an intrapulmonary mass relative to the mediastinum or chest wall in assessing for possible invasion.
We have found that the above sequences and modifications provide a robust set of tools to draw upon in answering most clinical questions. As always, a specific examination may require additional considerations, such as ECG-gating or an angiographic technique. It is becoming increasingly common for facilities to have default protocols and radiologists sitting in the reading room at a remote site. We believe it is important for the radiologist to evaluate the quality of the scan while the patient is still on the scanner as there are several opportunities to optimize or shorten the scan right at the console. Shortening the scan time can be particularly important for patients who are dyspneic, anxious, or who have trouble lying supine for a prolonged time, all fairly common occurrences in our patient population.
The scout is acquired as a free-breathing half-Fourier acquired single-shot turbo spin echo (Siemens HASTE) or single-shot fast spin echo technique (GE SSFSE). During this 25-s scan, 28 slices are acquired: 8 in the sagittal plane, 5 in the coronal plane, and 15 in the axial plane.
Series 2: Coronal T2 breath-held
In addition to its role as a screen for pathology, this series can be used as a reference for prescribing subsequent breath-held sequences. HASTE or SSFSE is typically the default sequence, allowing complete chest coverage in a single breath-hold. If further detail is desired, a 2D multislice multibreath-hold turbo spin echo (Siemens TSE) or fast spin echo (GE FSE) can be employed. We currently use a periodically rotated overlapping parallel lines with enhanced reconstruction (PROPELLER) technique acquired in about 5-6 breath-holds of about 17-23 s. BLADE is the Siemens proprietary variant of PROPELLER. We have found that the central k-space oversampling and inherent motion correction properties of this technique result in less motion artifact from the heart and subtle respiratory modulations as well as increased sharpness of the lung/pleural interface. Analogous observations in the pelvis have been reported. [8] Radial artifacts can be minimized by appropriate attention to blade width and oversampling parameters.
Series 3: Coronal 2D bSSFP, free-breathing
This series is a nonfat-saturated 2D multislice balanced steady state free precession (bSSFP) sequence. These image acquisitions are often extremely useful, providing exquisite anatomic information and soft tissue contrast as well as dynamic information on diaphragmatic excursion with respiration. Occasionally, relative tumor mobility can be assessed on these image acquisitions. This 2D technique of evaluating lung motion in both healthy volunteers and in patients with intra- and extra-pulmonary disease has been compared with other investigational 3D MRI techniques [9] with reported good correlation. In patients who cannot receive intravenous gadolinium, bSSFP images often provide an adequate look at the central vascularity.
Series 4: Navigator scout
The purpose of this series is to optimize placement of a 2D navigator for subsequent navigator-triggered acquisitions. Navigator Scout images are HASTE/SSFSE acquisitions, which, at first glance, may seem like a redundant series to the Scout Series. We have observed that: (1) initial anxiety can lead to erratic diaphragmatic motion, which is generally allayed this far into the examination, making tracking of the right hemi-diaphragm more regular at this point of the examination, and (2) we can obtain a more reliable location of the posterior aspect of the dome of the liver on an axial slice, which is an optimal place for navigator placement. Some patients who have had surgery on the right side may have suboptimal right hemi-diaphragmatic excursion, and in those instances, we have been successful in placing the navigator on the left hemi-diaphragm at the level of the spleen.
Series 5: Axial T2 navigator-triggered
We have found T2 TSE BLADE/PROPELLER to be qualitatively comparable to, if not favored over, conventional T2 TSE acquisitions, particularly given the reduced sensitivity to cardiac motion and increased sharpness of the major tissue interfaces. Fat saturation is routinely employed for this series. In addition to lesion characterization, this sequence is highly useful for the evaluation of lymphadenopathy and regional bone marrow signal.
Series 6: Axial diffusion-weighted imaging, respiratory-triggered
For this 2D multislice echo planar imaging (EPI) respiratory-triggered acquisition, we have selected b values of 0, 100, and 800 s/mm 2 . Diffusion-weighted imaging (DWI) in other body systems has provided information suggesting the cellularity of the lesion of interest and, because of this, is of particular interest as a potential biomarker of disease and treatment response. To obviate any T2* effects that could be induced in the lesion due to gadolinium, we have decided to perform DWI prior to contrast administration. Further investigation is needed to determine if "pseudoperfusion" (intravoxel incoherent motion) effects elucidated by using lower b-values (less than 100 s/mm 2 ) provide additional clinically relevant information.
Series 7: Pregadolinium T1 3D SPGR
A variety of 3D T1-weighted fat-saturated gradient recalled echo (GRE) sequences are available. Currently, we use a 3D spoiled gradient recalled (SPGR) with accelerated parallel imaging acquisition technique (Siemens VIBE with CAIPIRINHA or GE LAVA-Flex with Auto-calibrating Reconstruction for Cartesian (ARC) sampling and Dixon method for fat suppression, repition time/echo time TR/TE (3.82/1.8 ms), and matrix/slice thickness (256 × 256)/3 mm. In- and -out-of-phase images are routinely reconstructed. Homogeneous fat saturation of the anterior-superior mediastinum near the origin of the great vessels can be challenging with non-Dixon methods and particular attention to manual shim boxes is helpful in this regard.
Series 8: Test bolus
For this portion, repeated real-time single-slice GRE axial acquisitions at the level of the pulmonary artery are acquired following injection of 1 cc of intravenous contrast followed by a 20 cc normal saline flush. The time to peak enhancement in the pulmonary artery or ascending aorta can be determined.
Series 9: Postgadolinium T1 3D SPGR
Using the information from the test bolus, the initial postgadolinium series is timed such that peak arterial enhancement coincides with the time of central k-space filling. Identical parameters are used for the pre- and postgadolinium series, with images typically acquired in the axial plane. Subsequent postgadolinium images are typically obtained at 1, 3, and around 5 min. An additional imaging plane, either coronal or sagittal, is often obtained.
Series 10 (optional): T1 SPGR breath-held In- and out-of-phase
The information provided by this dual-echo 2D GRE sequence with respect to the presence of intravoxel fat is particularly useful in imaging anterior mediastinal masses where the normal or hyperplastic thymus is a consideration. [10] The imaging parameters are Repetition Time/First Echo Time/Second Echo Time (TR/TEΉ/TE) (170/2.38/4.76 ms), matrix/slice thickness (256 × 192)/5.5 mm. In practice, we have found the in- and out-of-phase images obtained from the pregadolinium T1 3D SPGR with Dixon technique can be comparably used, thus saving the time associated with running a separate two-dimensional T1-weighted Gradient-Recalled Echo (2D T1 GRE) for this purpose.
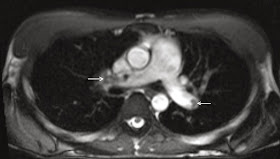
Series 11 (optional): Axial bSSFP breath-held
The 2D bSSFP (Siemens TRUE FISP or GE FIESTA) technique demonstrates T2/T1-weighting with high contrast and signal-to-noise ratio and can be obtained with rapid sequential acquisition, fat suppression, and overlapping thin sections. It is frequently used in cardiac and abdominopelvic MRI as a noncontrast-enhanced bright blood MR angiography/venography technique. These are typically performed as breath-held acquisitions but can be tailored to be free-breathing.
Series 12 (optional): Cine bSSFP
CinebSSFP (Siemens TRUE FISP or GE FIESTA) is a staple of cardiac imaging for the evaluation of cardiac wall motion, function, and valves. In the context of noncardiac chest MRI, this technique is useful for evaluating the motion of an intrapulmonary mass relative to the mediastinum or chest wall in assessing for possible invasion.
We have found that the above sequences and modifications provide a robust set of tools to draw upon in answering most clinical questions. As always, a specific examination may require additional considerations, such as ECG-gating or an angiographic technique. It is becoming increasingly common for facilities to have default protocols and radiologists sitting in the reading room at a remote site. We believe it is important for the radiologist to evaluate the quality of the scan while the patient is still on the scanner as there are several opportunities to optimize or shorten the scan right at the console. Shortening the scan time can be particularly important for patients who are dyspneic, anxious, or who have trouble lying supine for a prolonged time, all fairly common occurrences in our patient population.
No comments:
Post a Comment