Stroke is a serious condition that affects 25 in 100,000 newborns and 12 in 100,000 children under 18 years of age. It is the sixth leading cause of death in children. There are three types of stroke: arterial ischemic stroke, sinovenous thrombosis, and intracranial hemorrhage.
-->
Acute "Pediatric Stroke MRI "
- DWI in three planes and calculated ADC map
- Coronal FLAIR
- Axial T2-W FSE
- Sagittal T1-W SE
- Intracerebral 3-D TOF MRA
- Axial dual-echo STIR and T1-W spin-echo through the neck
- Extracerebral 2-D TOF MRA of the neck down to the aortic root
Non-acute "Pediatric Stroke MRI"
- Acute stroke protocol without imaging of the neck
Teaching points of "Pediatric Stroke MRI"
The aims of conventional MRI are not only to detect the infarct, but also to provide information to establish the cause of the stroke and to exclude other causes (such as tumour or infection). The majority of children with stroke have a combination of risk factors including sickle cell disease, congenital heart disease, anaemia, prothrombotic disorders and infections such as varicella-zoster . The rationale for the inclusion of intracranial MRA in all children with stroke is that cerebral arteriopathy is found in up to 80% of these children and most commonly affects focal areas of large intracranial arteries . Specific entities such as moyamoya disease may also be diagnosed. The commonest abnormality identified is occlusion or stenosis, of unknown aetiology, affecting the terminal internal carotid artery (ICA) or proximal middle cerebral artery (MCA).
Extracranial MRA and, either a dual-echo STIR or fat-saturated axial T1-W imaging, through the neck can detect arterial dissection, particularly in children with posterior circulation infarcts . The inversion time of the STIR sequence is selected to suppress the fat within the neck. The fat saturation provided by both these sequences improves the conspicuity of the haematoma within the extracranial vessel wall.
A 3-D TOF MRA sequence is used for the imaging of the intracranial vessels and a 2-D TOF MRA sequence for the extracranial vessels. The TOF scan times are shorter than phase-contrast (PC) MRA and there is lack of dependence on the choice of correct velocity encoding with obvious advantages when scanning ill children. Intracranial 3-D TOF MRA is also included in the investigation of children with IPH, although its sensitivity to T1 shortening may obscure the underlying abnormality .
As CT is often the first-line investigation in children with stroke, the potential of DWI to detect hyperacute cerebral infarction prior to changes on T2-W MRI is not realized. However, inpatients (e.g. cardiac patients, patients with recent-onset stroke) can be imaged early, and in these children DWI can be used to detect infarcts of different ages.
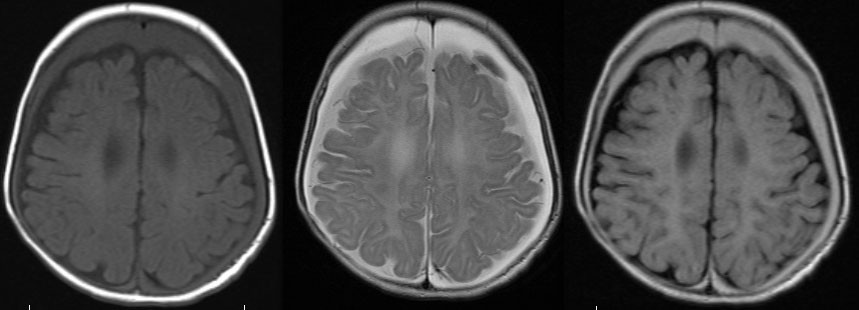
 a | The MRI reveals a small acute stroke that shows restriction on diffusion-weighted imaging in the periventricular region (arrow). b | The corresponding apparent diffusion coefficient map confirms the occurrence of acute ischemia (arrow). c | The perfusion-weighted image shows a large area of hypoperfusion—basically the entire left middle cerebral artery territory (arrows)—representing diffusion–perfusion mismatch. d | This stroke was caused by embolization of a cardiac thrombus that led to partial occlusion of the internal carotid artery—little flow is seen on magnetic resonance angiography (arrow)—and complete occlusion of the middle cerebral artery (arrowhead).
a | The MRI reveals a small acute stroke that shows restriction on diffusion-weighted imaging in the periventricular region (arrow). b | The corresponding apparent diffusion coefficient map confirms the occurrence of acute ischemia (arrow). c | The perfusion-weighted image shows a large area of hypoperfusion—basically the entire left middle cerebral artery territory (arrows)—representing diffusion–perfusion mismatch. d | This stroke was caused by embolization of a cardiac thrombus that led to partial occlusion of the internal carotid artery—little flow is seen on magnetic resonance angiography (arrow)—and complete occlusion of the middle cerebral artery (arrowhead).



No comments:
Post a Comment