Without contrast FOOT MRI Sequences
- AX (LONG AXIS) T1
- AX (LONG AXIS) STIR
- COR (SHORT AXIS) STIR
- COR (SHORT AXIS) T2
- SAG STIR
- SAG T1
- THIN SLICE AXIAL PD FAT SAT
POST CONTRAST FOOT MRI
GAD- COR FMPSPGR FAT SAT PRE/POST GAD
POSITIONING of the Patient for FOOT MRI
- Prone and foot is plantar flexed (Preferred Method)
- Supine and toes sticking out of coil (Alternative Method)
TECHNICAL NOTES
The foot and ankle are among the hardest of all areas to image because of the complex three-dimensional anatomy. Magnetic resonance imaging (MRI), with its multiplanar capabilities, excellent soft-tissue contrast, ability to image bone marrow, noninvasiveness, and lack of ionizing radiation, has become a valuable tool in evaluating patients with foot and ankle problems. MRI is more specific than bone scintigraphy and provides more information than ultrasound and computed tomography. Arthroscopy of the ankle is limited to the articular surface and joint space. MRI allows a global evaluation of the bones, tendons, ligaments, and other structures with a single examination that exceeds the capabilities of all other available techniques. This monograph was written to provide a useful guide to basic technique, indications, positioning, anatomy, and interpretation of foot and ankle MRI. The first part describes the performance of the MRI examination with reference to the positioning of the foot, types of coils, and advantages and disadvantages of the different sequences and imaging planes. The next section was written by an experienced foot and ankle orthopedic surgeon and outlines the indications for MRI for the common foot and ankle symptom complexes and the information that the surgeon hopes to obtain from the study. This is followed by a review of pertinent anatomy, as it applies to imaging, with emphasis on osseous structures, ligaments, tendons, and muscles. The final section is a comprehensive review of the common pathologic conditions encountered in the foot and ankle. We hope that radiologists and radiologists-in-training find this article a useful reference tool and gain a better understanding of this complex area of musculoskeletal imaging.
READ MORE:
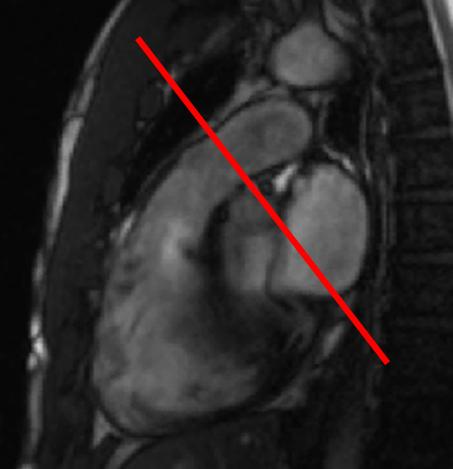
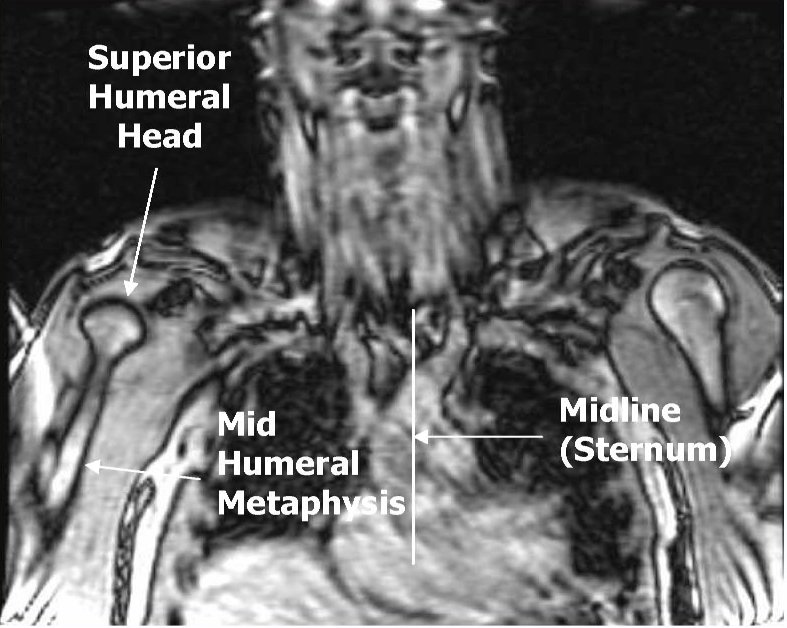
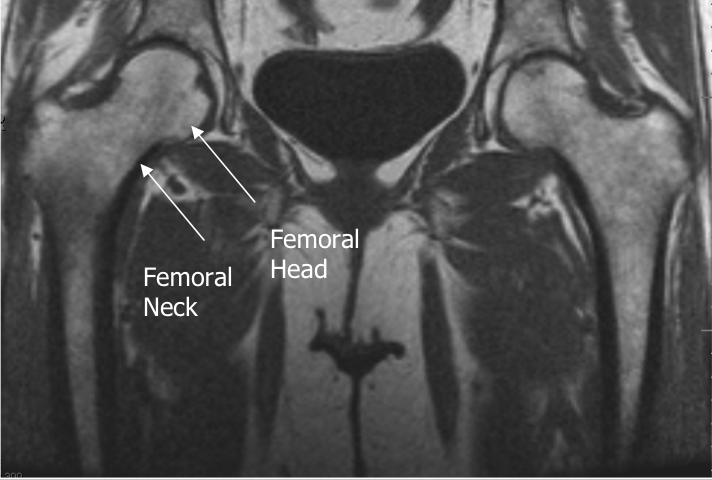
Foot MRI Reference Lines